International Hepato-Pancreato-Biliary Association
Education
Online Educational Platform - myHPB
myHPB is an innovative elearning platform providing IHPBA members with up-to-date, quality-assured content, including master class videos and key educational resource as well as a meeting space to discuss the latest developments in our specialty field.
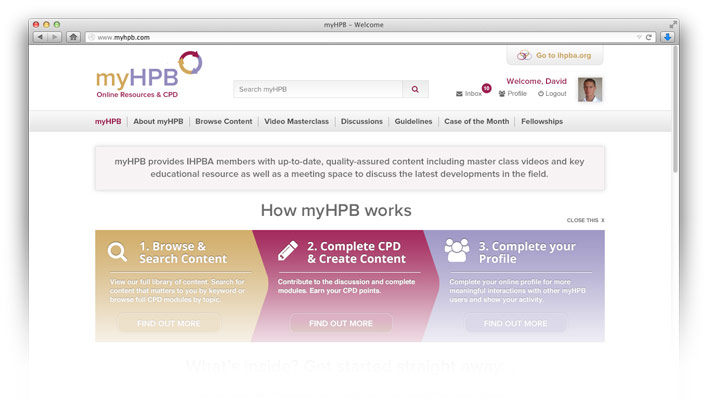
This platform has been developed to facilitate access to the highest quality learning resources and to enable interaction with like minded individuals
Join IHPBA and benefit from this innovative resource!
Try myHPB NOW Membership benefits
Education and Training Committee Projects
Pre-Operative Planning Modules
(The full catalogue of pre-op planning modules are availalbe to members on myHPB, you will need to be logged in as a member for the link above to work).
Login into myHPB
Corporate Partners
If you are interested in becoming a Corporate Partner of the IHBPA please contact industry@ihpba.org
Find out more


